Case study 1
Unexplained dyspnea in a 46-year-old female
Kate is a 46-year-old woman who presented with unexplained dyspnea.
-
She had been otherwise healthy until about 4 years ago, when she noted gradual onset of dyspnea with exercise
-
She presented with no associated symptoms
-
Kate attributed her shortness of breath to weight gain
She visited her PCP, and she ordered a chest x-ray, pulmonary function tests (PFTs), and blood work. These were reported as being normal.
-
Kate was referred to a cardiologist. An echocardiogram was performed, and it demonstrated mild right enlargement of the right ventricle (RV) and an RV systolic pressure (RVSP) estimated at 45 mmHg
-
The cardiologists told Kate to lose weight and exercise more
Kate’s dyspnea persisted, so she was referred to a pulmonologist.
-
The pulmonologist reviewed the echo, was concerned, and referred Kate to another cardiologist for right heart catheterization (RHC)
-
The cardiologist ordered a CT scan. The report said,
-
-
“No evidence of PE. Pulmonary artery enlarged. Lung parenchyma normal.”
-
-
PFTs were repeated, demonstrating normal volumes and flows. Carbon monoxide diffusion in the lung (DLCO) was 58% of predicted
Kate then underwent RHC:
-
Right atrial pressure was 4 mmHg
-
Pulmonary arterial pressure (PAP) was 52/24 mmHg, mean 33 mmHg
-
Cardiac output was 4.8 L/min
-
And her pulmonary vascular resistance (PVR) was 6 Wood units (or 480 dyn∙sec∙cm-5)
Kate was started on drug treatment for pulmonary arterial hypertension (PAH, WHO Group 1).
-
After 4 months of treatment, she had not improved significantly
-
Repeat echocardiogram showed continued RV enlargement and unchanged RVSP
Kate’s CT
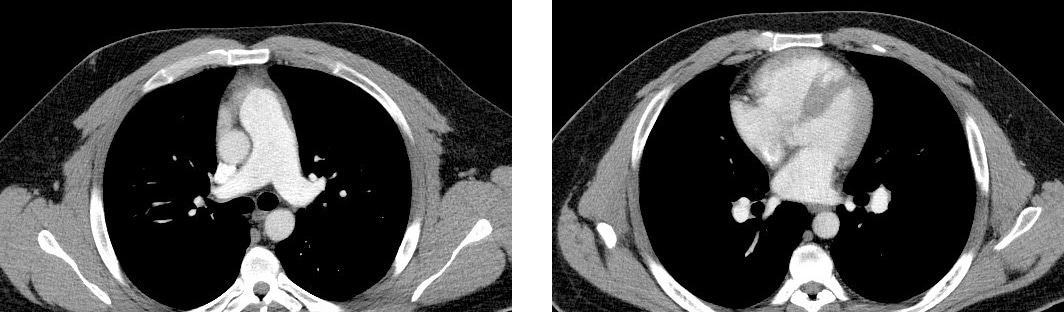
Though Kate had had a CT scan, she had never been given a ventilation/perfusion (V/Q) scan to rule out chronic thromboembolic pulmonary hypertension (CTEPH, Group 4).
According to the World Symposium on Pulmonary Hypertension and largely based on findings reported by Tunariu et al (2007), CT pulmonary angiography has a sensitivity of only 51% for CTEPH, compared with the V/Q scan’s sensitivity for CTEPH of 96% to 97%.1 That’s why the V/Q scan is the preferred and recommended screening tool for CTEPH.2
Kate’s V/Q scan
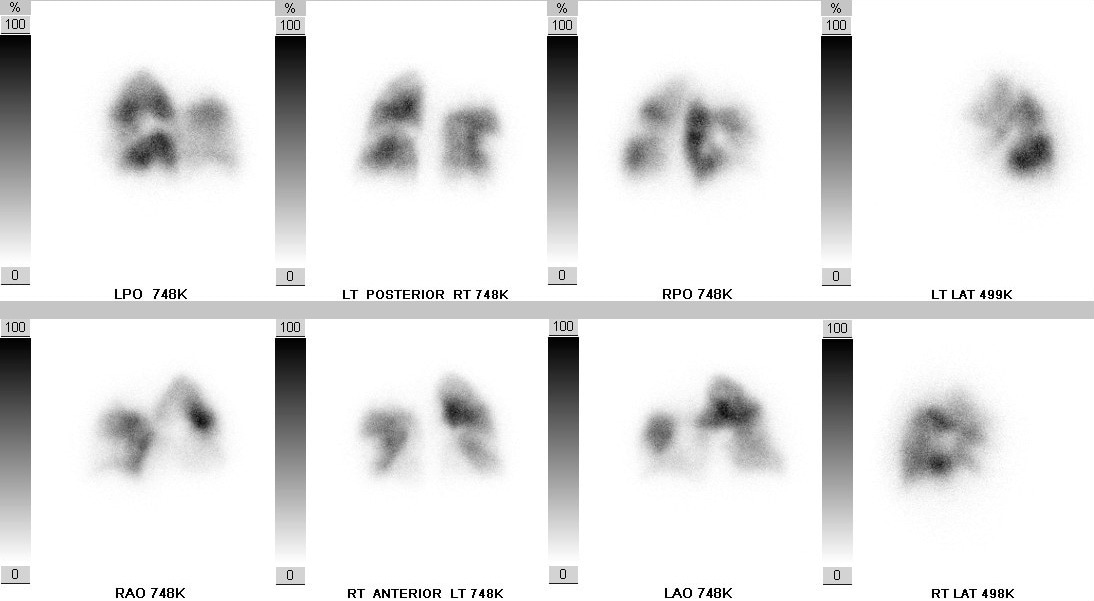
After her V/Q scan was evaluated, Kate was referred to a CTEPH center.
-
Pulmonary angiography was performed, and it showed that Kate had bilaterally accessible CTEPH disease
-
She underwent pulmonary thromboendarterectomy (PTE) surgery
-
Her recovery was unremarkable
-
6 months after surgery, she has normal exercise capacity and her echocardiogram is normal
Key learnings
Patients diagnosed with CTEPH do not always have a history of a diagnosed acute pulmonary embolism (PE): Estimates of the number of CTEPH patients who present without a history of acute PE range from about a quarter to almost two-thirds3,4
On average, there is a delay of well over a year in diagnosis of CTEPH3,5
A CT scan may show CTEPH disease, but it may be unremarkable
The V/Q scan is more sensitive than CT for CTEPH, and it is the preferred and recommended screening test for CTEPH1
References:
1. Tunariu N, Gibbs SJR, Win Z, et al. Ventilation–perfusion scintigraphy is more sensitive than multidetector CTPA in detecting chronic thromboembolic pulmonary disease as a treatable cause of pulmonary hypertension. J Nucl Med. 2007;48(5):680-684. 2. Kim NH, Delcroix M, Jenkins DP, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62(suppl D):D92-D99. 3. Pepke-Zaba J, Delcroix M, Lang I, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation. 2011;124(18):1973-1981. 4. Lang IM. Chronic thromboembolic pulmonary hypertension–not so rare after all. N Engl J Med. 2004;350(22):2236-2238. 5. Held M, Grün M, Holl R, et al. Chronic thromboembolic pulmonary hypertension: Time delay from onset of symptoms to diagnosis and clinical condition at diagnosis. Dtsch Med Wochenschr. 2014;139(33):1647-1652.


