Case study 2
A case of “failure to recover” from pulmonary embolism (PE)
Jack is a 56-year-old orthodontist with a history of deep vein thrombosis (DVT) 12 years ago.
-
He was treated with anticoagulation for 3 months
-
8 years ago, Jack developed an acute pulmonary embolism (PE) after a long flight
-
Jack was started on anticoagulation subsequent to the PE, and he has been on it ever since
Jack’s HCP notes that Jack never completely “recovered” from the PE.
-
He has persistent exercise intolerance
-
Occasional palpitations and chest pressure—but no syncope
-
His father had DVT; otherwise, no meaningful family history
Jack’s past medical history includes systemic hypertension and mild arthritis.
-
He’s on an ACE inhibitor, warfarin, and a beta blocker
-
16 years ago, he had a knee arthroscopy but has had no other surgeries
On physical exam, Jack appeared generally well.
-
His lungs were clear, though a murmur was heard over the left posterior lung field
-
His heart showed a II/VI holosystolic murmur along the left lower sternal border and a somewhat loud P2
-
He had no edema or clubbing
On referral, initial evaluation of Jack revealed the following:
-
Chest x-ray showed mild cardiomegaly and clear lungs
-
Chest CT showed mosaic perfusion and potential irregularities of the right descending pulmonary artery; no luminal filling defects were evident
-
Echocardiogram showed moderate right ventricular (RV) enlargement and dysfunction
-
RV systolic pressure was estimated to be 64 + right atrial pressure
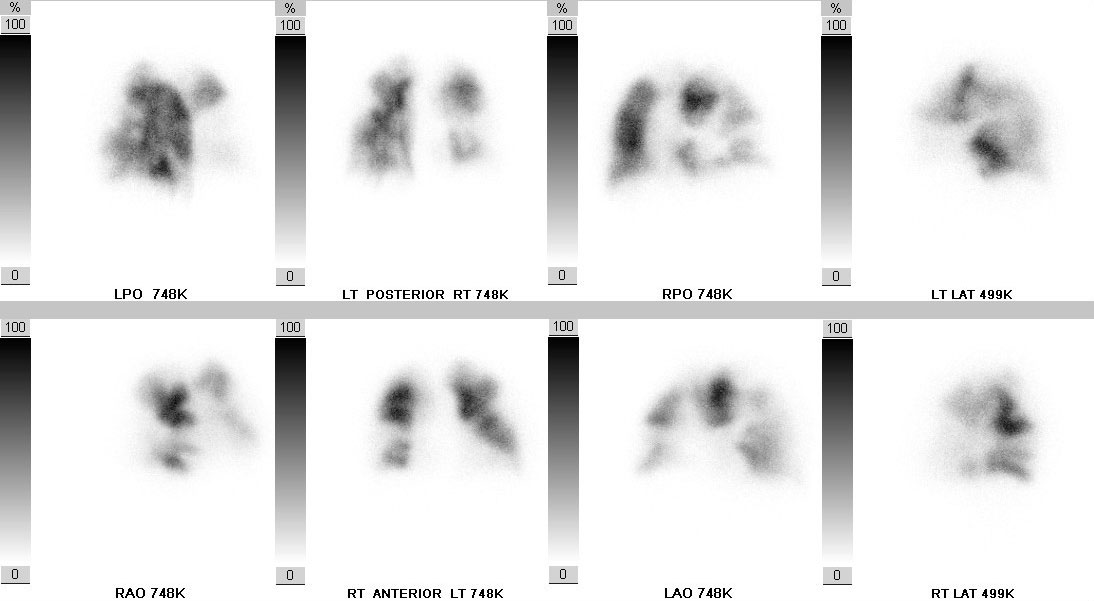
Segmental map

There are evident defects on Jack’s ventilation/perfusion (V/Q) scan
Key learnings
Failure to symptomatically return to baseline after an acute PE should raise suspicion for CTEPH1
V/Q scanning is highly reliable and should be ordered promptly2
Bilateral large defects are typical in surgically accessible CTEPH
Referral to a CTEPH center (several throughout the US and Europe) is recommended when CTEPH is suspected2
References:
1. McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension. Circulation. 2009;119(116):2250-2294. 2. Kim NH, Delcroix M, Jenkins DP, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62(suppl D):D92-D99.


